Series of Facebook posts by Thedra Cullar-Ledford
Drawing the Eye to Nothingness
G Gallery, Houston
April 2015
December 14, 2013
It’s amazing how things can change.
Yesterday morning, I was getting ready to donate a kidney. I had been through test after test, waiting for the donation chain to come together. There was one final request from the clinic that was to receive my kidney — for a mammogram. I hadn’t had one for years, so the hospital arranged one on short notice.
I’m not giving a kidney anymore because I have (what appears at this point to be) ductal carcinoma in-situ aka “stage zero” breast cancer. We’ll do a biopsy in a few weeks and then figure out what to do, but my expectation is that I will be getting a complete boob job pretty soon. I feel really sad that I can’t donate, and that I broke the chain that would have helped so many people. I hope they can put it back together soon.
January 7, 2014
I have a bit more information about my boobies based on last week’s biopsy.
It appears that the initial thinking — that it is DCIS — is correct. There is also a small spot of an invasive cancer, but the fact that it is there does not change the treatment plan. Next step is to meet with the plastic surgeon and to do the BRCA genetic test. Once we have that result, we’ll meet with the medical oncologist.
It sounds like surgery is several weeks away at the soonest, but there is not a firm schedule yet. I feel better now that we seem to be moving forward with a plan. It’s all very Angelina Jolie. Rock on!
January 13, 2014
Met with the oncologist today who had more info from the biopsy last week.
New diagnosis is “invasive ductal carcinoma.” Again, the invasive part does not really change the treatment plan compared to “ductal carcinoma in situ.” The difference is that some of the naughty little cells have escaped their cozy ductal home. There is no evidence that any of them have made it to a lymph node yet (which is good.) This is one of the things we will find out during surgery and in the week or so after.
Apparently us breast cancer patients are lucky because research has figured out how to identify different types of breast cancers. Mine is being stimulated by estrogen & progesterone. This is also good because there are medications that interfere with this mechanism. My cancer is also a very slow-growing type. I’m not likely to need chemo or radiation.
In any case, the left one is a goner. It will mostly be up to me whether or not to have a matching set installed. In most cases, the reconstruction procedure occurs several weeks or months after the mastectomy procedure, so that if they need to do something else to get the cancer they don’t ruin the brand new tits.
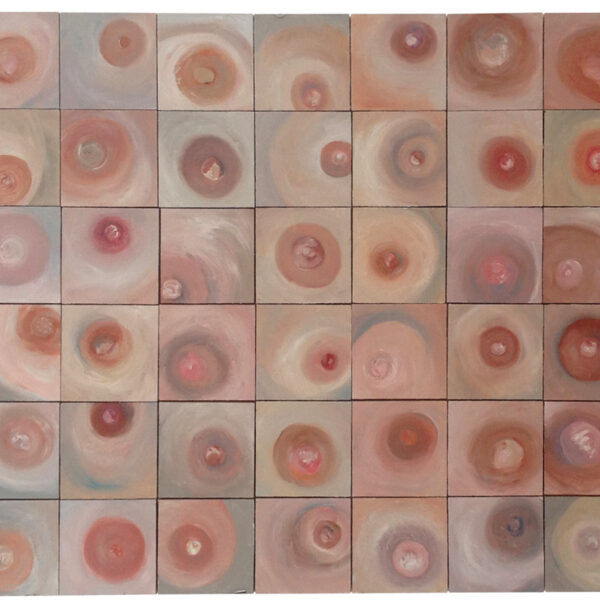
Shocking fact: one in eight women will be diagnosed with breast cancer. About 90% of those are from complete randomness. The other 10% are hereditary cases where both the BRCA1 and BRCA2 genes are malfunctioning. We do not yet have my BRCA genetic test results back, but I am likely negative.
Everyone please go have your tits squeezed by a professional for me. (And then later by someone you like!)
Ending with a quote from my good friend B Moody: “This is all such a fucking bore!”
January 22, 2014
Met with plastic surgeon today. I decided to do both to keep things symmetrical. Surgery likely in about a month. During the mastectomy surgery, he will put “expanders” under the pectoral muscles. A few weeks later, these can gradually be inflated until they get to the size I want (not very big.) Then comes another, smaller surgery to remove the expanders and install the final implants. Decoration (nipple tattoos etc) will be sorted out after all that is done.
January 30, 2014
I had a consultation with the genetic counselor last week. I already had the BRC-A and BRC-B test (both negative), but they really want to figure out why my body manifested so much cancer, seemingly out of nowhere.
There are additional genetic tests which they would like to do. While a positive BRC-A test explains about 10% of all breast cancers, these other tests have much smaller predictive abilities.
I guess genetic counseling is required because these tests can tell you things that you and your family might not want to hear or know. These issues are not very important to me because a) I already had breast cancer, and b) I only gave birth to males. I agreed to the tests because they won’t cost me anything more (we have already maxed out our annual deductible) and maybe my results will help with the scientific research.
We also met with Dr. Rodriguez, the oncologist. He had results back from the genetic type tests on some of my tumors. The question, in my case, is whether all of the cancers found are of the same type. If they are all the same, non-aggressive types, then further treatments are not necessary. The first two tumors they tested (the two largest ones) were the same — not aggressive. They are testing a few more now and we’ll get those results back in a few weeks.
The guidance, therefore, is not to prescribe chemotherapy or radiation therapy, since neither improves the final outcome any more than doing nothing. I was very happy to hear this.
He will prescribe Tamoxifen, a drug that blocks the female hormones progesterone and estrogen. Those hormones were spurring my cancers to grow, and blocking them will shut down that mechanism. There are potentially side-effects, including the early and sudden onset of menopause. I had a hysterectomy a few years ago and there was some confusion afterwards whether or not the ovaries were taken out too. I need to find out if I still have ovaries because that will make a big difference. Stephen is looking for his snorkel.
When you are about to go nuts and aggravated and in pain and sick if the poking and waking up and the trying to sleep and the noise and the light, remember we ALL Love you, and not that little sniveling kind of Love, we Love you with a BIG Love that is wonderful and abiding and mysterious and powerful. Because you are bigger than all this crap around you…. and this will pass. And Stephen is your brilliant knight who we Love equally. We are all out here pulling and crying and praying for you my darling. I promise, we are. I promise. from one cancer survivor to another. I promise.
Michelle Marie Engelman Berns
February 17 – 20, 2014
Removal operation complete, now starting reconstruction operation (two more hours.) All going well so far. No indication of cancer in lymph nodes, which is excellent news. Thanks to everyone for all the nice notes!
Thedra is now out of surgery and in recovery. The rest of her procedure was normal. All in all, the day has gone better than expected.
It took a long time to get released from the hospital, but Thedra is home now. She’s uncomfortable and impatient, but that’s to be expected. We’re trying to get her ‘nest’ properly constructed and medicine routines figured out. She would love visitors, though she sleeps a lot. Again, thanks for all the well-wishes! We have the best friends anyone could hope to have.
February 26, 2014
Had two appointments yesterday, first with the plastic surgeon (yawn), then with the primary surgeon (wow!)
You may remember that I decided to have both boobs chopped off to stay symmetrical, even though only the left one was a troublemaker. It turns out that the right one was not nearly as innocent as it had been pretending to be. It had been harboring DCIS, some LCIS, a little ADH, and a dash of ALH/LCIS. All of these are different forms of cancers, though none of them are invasive. It was a Whitman’s Sampler box, “totally* full” of cancers that surprised all of my doctors.
As for the left one, they didn’t find three tumors they expected, but they found seven (!) ranging from 1 cm to 1.95 cm in size. They also found quite a bit of DCIS, but we knew that was coming.
While all of this could have been very bad news, there are three very important, and very good things that made yesterday a great day. First, I had both boobs removed (I’m the kind of girl who like matching bedside tables.) Second, none of the lymph nodes on either side have any cancer in them at all. Since the lymph nodes are how cancer spreads throughout the body, this means that it has not spread. Finally, no cancer was found around “the margins” of the surgery area. In other words, it appears that they got all of it.
The big question to be answered now is whether or not chemo will be needed, and there is not an obvious answer at this point. They are going to do more analysis of all the tumors, and genetic testing of several of them to find out if they are all of a similar, well-behaved and unaggressive type. If so, then chemo is unlikely. If, however, there is even one of the little fuckers that is aggressive, the decision becomes trickier. We’ll know more in a couple of weeks.
Tumor Board Discussion
The focus of the debate had to do with how to “stage” my cancer. There are two ways of doing that assessment: by the size of the largest tumor (1.9 cm) or, by the total size of ALL the tumors (over 6 cm.) If they use the first approach, I have “stage one” cancer that would not require chemotherapy. If they use the second approach, I have “stage two” cancer that does require chemotherapy.
The winning argument seems to be that a large tumor behaves very differently from a small tumor. It is large because it is more aggressive. Small tumors, especially my slow-growing kind, aren’t doing that. They have therefore staged my cancer at stage one, but they are submitting samples of my largest tumors for a complete genetic workup. The expectation is that all of the tumors are of the same type, but the genetic test will determine that.
In other words, once I have this next surgery, I’m done with my cancer odyssey. I will have to take Tomoxafin for the next ten years to block progesterone and estrogen (which was feeding my cancers), but the primary side-effects of that drug shouldn’t effect me too badly.
Believe it or not, yesterday was a freaky and fantastic day, full of crazy and wonderful chance encounters and meaningful conversations.
Thanks to all of you!
(* actual word the doctor used.)
February 26, 2014
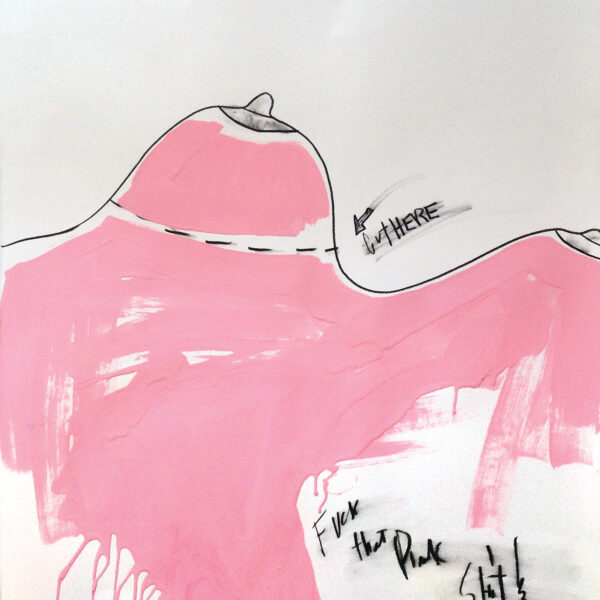
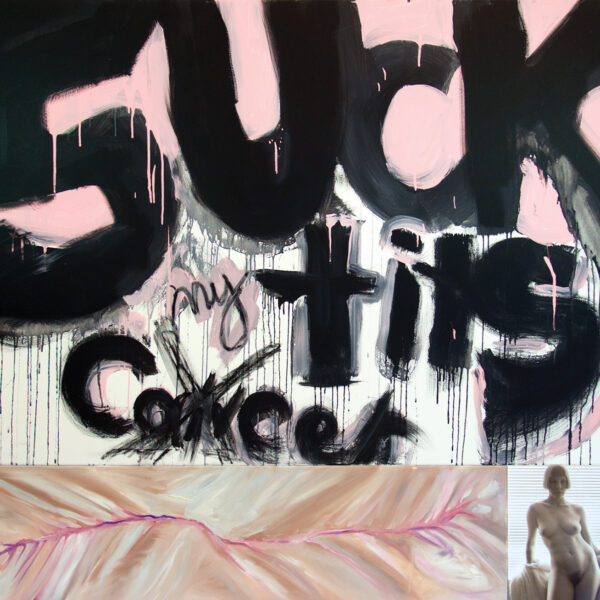
If my plastic surgeon had spent ten more minutes getting to know me I would have never gone with reconstruction. He kept arguing with me and saying ”you‘ll be concave.“ I kept saying that I just wanted to be flat. Since this was all being provided for free, I felt compelled to be quiet, and to go along with what he wanted to do. I finally said ”OK, just an ‘A.‘“
In the week and a half after surgery, I learned that there would be no nipple, there would be no feeling, that it can take six or even nine procedures to finish reconstruction, that implants can hide new tumors, and that you have to replace them every 10 years.
Why, when they just removed cancer from your body, would you want to have some PLASTIC put right back in there? Hmmm, what’s a common carcinogen?… PLASTIC?
I equate it to this: My son has died, lets stuff him and prop him up in the corner so that nobody else notices that he’s gone. Why all this trouble so that society can be happy thinking that nothing had ever gone wrong?
I knew going in to my follow-up appointment with my plastic surgeon that he was not going to like what I was planning to tell him, so I recorded it. We’ve only been able to listen to this once because it upsets my husband and I so much.
I now know that my experience was not uncommon. Dealing with how fucked up that is will be a whole other body of work.
March 10, 2014
About three weeks post surgery, I started to develop an infection in the left one that was causing not only pain, but weakness and dizziness. On Friday, the plastics doctor asked me to go into the ER at Methodist, not because I had an emergency but because that was the easiest way for them to get a good look at me.
The ER doctor still had to check me out. He pretty much only wanted to make sure I wasn’t dying right then, but then we started talking. He enjoyed the whole kidney/finding cancer story, but wasn’t all that surprised. He said that in the normal course of treating emergency cases he finds cancer two or three times a month that the patients didn’t know they had.
Miscommunication among the ER, my surgeon, and the plastics doctor meant that my surgeon, Dr. Bass, was the first one to show up. I think she was concerned that the drains were causing more harm than good. Though the drains were still removing fluids that needed to come out, the plastic tubes also offered a pathway for infection. She decided to remove the drains, even though the plastics doctor was the one responsible for them. I felt better.
When the plastics resident finally arrived at the ER (he had been sitting around waiting for the call for hours) he seemed to have concerns about the drains being removed. A few hours afterwards, we got a call from the plastics doctor’s nurse telling us to be very, very vigilant over the weeked about potential problems. We should immediately go to the ER if we saw any of these symptoms. She scheduled an appointment early Monday morning.
Over the weekend, we did notice these symptoms and called in to find out whether an ER visit was necessary. The on-call doctor said to stay at home both times.
March 12, 2014
Monday morning, as instructed, I drove out to Katy to have my appointment with the plastic surgeon. They were concerned about infection, and I was not feeling well. After examining me, he decided to do the second surgery, to remove the expanders, the next morning.
We got all our paperwork and were headed out to the car when I basically collapsed. I couldn’t make it to the car, let alone to home overnight. A kind nurse who was walking by noticed and escorted me to the emergency room and got some fluids into me. She arranged to have me admitted immediately.
The room was four star! Corner suite with nice windows and a seperate room for Stephen to sleep in. (He really needed it — we had stayed up all night watching for infection and nursing me through.)
In the morning, I had the surgery which went very smoothly. The painkillers worked well and the recovery was much easier. I was up wandering around the next day. I immediately felt like the toxic shit had been removed.